 Dr. Lior Rennert, Director
Dr. Lior Rennert, Director
Dr. Lior Rennert is an Associate Professor of Biostatistics in the Department of Public Health Sciences at Clemson University. He received his PhD degree in Biostatistics from the University of Pennsylvania’s Pearlman School of Medicine and his MS degree in Statistics from the University of Chicago. His work focuses on the development and application of statistical and mathematical models to guide health-related decision making in the health sciences. Currently, Dr. Rennert and his team are developing an epidemiological modeling framework to identify communities at high-risk for opioid-use disorder, hepatitis C virus (HCV), human immunodeficiency virus (HIV), and respiratory infectious diseases, including Covid-19. The ultimate goal of this project is to develop a toolkit to help inform decision making for resource allocation to medically underserved and at-risk communities. As Clemson University’s Lead Public Health Strategist for Covid-19, Dr. Rennert and his team have developed models that helped guide university policy throughout the Covid-19 pandemic. He also works closely with Prisma Health’s Opioid Stewardship Program to evaluate opioid-related policies on patient well-being. Dr. Rennert has formed partnerships with several organizations statewide, including Prisma Health, Clemson Rural Health, The University of South Carolina’s Center for Rural and Primary Health Care, the Medical University of South Carolina, and South Carolina’s Department of Health and Environmental Control.
Center for Public Health Modeling and Response
The Center for Public Health Modeling and Response aims to utilize data-driven approaches to inform clinical and public health decision-making and assist the ability of health organizations and communities to prepare for, and respond to, public health threats.
-
Overview
Purpose
Our purpose is to improve health outcomes for communities across South Carolina by creating usable knowledge for public health decision makers. Through a dedication to education, research, and service, we aim to train the next generation of public health modelers to develop and implement data-driven approaches to inform and assist clinicians, health organizations, and communities on public health response.Justification
There is a public health need to utilize data-driven approaches to inform patient care and community needs. Modeling frameworks are being designed and implemented to help healthcare professionals, patients, and public health implementors with decisions about diagnostic testing, treatment initiation, lifestyle changes, and resource allocation. Such models are especially useful because they can provide objective data on the decision-making process and help avoid biases observed in clinical and public health decision making.Vision
Our vision is to be a leading resource for usable knowledge for public health decisions makers. -
Our People
Director and Staff
 Dr. Kerry Howard, Research Manager
Dr. Kerry Howard, Research Manager
Dr. Kerry Howard is the Research Manager at the Center for Public Health Modeling and Response. She received her PhD degree from Clemson University in Applied Health Research and Evaluation and a MS degree from Seton Hall University in Experimental Psychology and Cognitive Neuroscience. Her research focuses on the elimination of health disparities through data-driven examinations of delivery of care in disadvantaged populations, as well as methodology that impacts decision-making in the prevention and treatment of cognitive decline and Alzheimer’s Disease, opioid use disorder, Hepatitis C, and community child safety. Dr. Howard has performed research in the fields of health and psychology over the course of her career, accumulating extensive experience with research design, data maintenance and analysis, and scientific writing, as well as an understanding of how these areas can be applied to improve real-world outcomes and disseminate findings to the community. Karen Atkinson, Administrative Coordinator
Karen Atkinson, Administrative Coordinator
Karen Atkinson is the Administrative Coordinator for the Center for Public Health Modeling and Response and Research Program Manager within the Department of Public Health Sciences. She received her MS from Furman University in Exercise Physiology. She has contributed to various projects for the CDC, DoD, USAID, NIH, AHA, and many others as well as managed budgets of a combined total of $30M. She has performed research in the fields of high obesity prevention, mobile health, remote patient monitoring, diabetes prevention, and rural health. Dr. Tolulope Fashina, Program Manager, DMA-PRIME
Dr. Tolulope Fashina, Program Manager, DMA-PRIME
Dr. Tolulope Fashina is the program manager for the CDC-funded grant, “Disease Modeling and Analytics to inform Outbreak Preparedness, Response, Intervention, Mitigation, and Elimination in South Carolina (DMA-PRIME).” She received her MD degree from All Saints University School of Medicine, Dominica, and an MPH and Certificate in Global Health from Johns Hopkins University School of Public Health. Dr. Fashina has worked in research and research management in global health and infectious disease throughout her career, most recently overseeing clinical trials as the clinical research supervisor at the University of Nebraska Medical Center. Dr. Jiande Wu, Data Manager/Data Scientist
Dr. Jiande Wu, Data Manager/Data Scientist
Dr. Jiande Wu is the Data Manager/Data Scientist at the Center for Public Health Modeling and Response. He received his PhD degree and MS from the University of New Orleans in Electrical Engineering. He also holds MS and BS degrees from North China Electric Power University in Computer Science and Engineering. Dr. Wu possesses extensive training expertise in the field of computational genomics and data analysis. His research primarily focuses on the development and application of advanced big data analysis techniques and computational genomic methods. Dr. Wu currently serves as the Center’s Data Manager and is responsible for data extraction and management of electronic health records (EHR) data. He is also responsible for overseeing the application of machine learning techniques for prediction, including the development of early warning systems for infectious disease outbreaks based on digital trace data. Dr. Fatih Gezer, Research Associate
Dr. Fatih Gezer, Research Associate
Dr. Fatih Gezer is a Research Associate at the Center for Public Health Modeling and Response. He received his PhD and his MS degrees in Statistics from the University of Leeds in the United Kingdom and the University of Delaware, respectively. He has expertise in Spatio-temporal statistics, spatial point processes, the statistical properties of the geometric structures obtained from points such as Voronoi tessellations, and denoising methods for noisy spatial data. His current research focuses on the application of statistical methods to public health through the mathematical modeling of infectious diseases, with a particular focus on rural and medically underserved communities. Dr. Jecinta Ibeji, Postdoctoral Fellow
Dr. Jecinta Ibeji, Postdoctoral Fellow
Dr. Jecinta Ibeji is a Postdoctoral Fellow in the Department of Public Health Sciences at Clemson University. She received her PhD and MS degrees from the University of Kwazuli-natal, South Africa in Statistics. Her expertise is in Bayesian spatiotemporal modeling of infectious diseases and disease mapping. Her role in the Center focuses on the application of statistical modeling for infectious disease mapping and epidemiology. Dr. Md Sakhawat Hossain, Research Assistant Professor
Dr. Md Sakhawat Hossain, Research Assistant Professor
Dr. Md Sakhawat Hossain is a Research Assistant Professor in the Center for Public Health Modeling and Response. He received his PhD from Texas Tech University in Statistics and MS degree from Clemson University in Mathematics. His expertise is in development of predictive modeling frameworks, parameter identification, and numerical optimization. His role in the Center focuses on development, optimization, and calibration of predictive modeling frameworks for infectious diseases. Dr. Brian Witrick, Assistant Professor
Dr. Brian Witrick, Assistant Professor
Dr. Brian Witrick is an Assistant Professor in the Department of Public Health at Clemson University. He received his PhD from Clemson University in Applied Health Research and Evaluation and a Master of Public Health from Armstrong Atlantic State University in Epidemiology. Dr. Witrick has expertise in spatial epidemiological methods, including small area estimation and spatio-temporal modeling. He has experience in research working to provide clinicians with the best evidence to support the care of patients with cardiovascular disease and in investigating racial disparities in maternal and infant health. His current research focuses on cardiovascular epidemiology and the use of spatial analysis to understand disparities, compare outcomes, and improve clinical practice in South Carolina. Mohammad Mihrab Uddin Chowdhury
Mohammad Mihrab Uddin Chowdhury
Mihrab will be joining the Center for Public Health Modeling and Response as a postdoctoral fellow in modeling. Mihrab has received an MS from University of Dhaka in Mathematics and will receive his PHD from Texas Tech University in Applied Mathematics. Mihrab has extensive experience in developing mathematical models and applying dynamical systems theory. His research interests include developing infectious disease models and employing machine learning for early detection of risk factors and preventive measures. GM Fahad Mostafa
GM Fahad Mostafa
Fahad will be joining the Center for Public Health Modeling and Response as a postdoctoral fellow in data science. Fahad has received an MD from University of Dhaka in Applied Mathematics and will receive his PhD from Texas Tech University in Statistics. Fahad has extensive knowledge machine learning, deep learning, and statistical analysis, including utilizing advanced machine learning methods for analyzing and forecasting disease patterns. He looks forward to using these skills to incorporating research findings into practical applications, such as the strategic deployment of mobile health clinics, raising community awareness, and developing statewide disaster simulation scenarios. Nusrat Tabassum
Nusrat Tabassum
Nusrat will be joining the Center for Public Health Modeling and Response as a postdoctoral fellow in modeling. Nusrat has received an MS from University of Dhaka in Mathematics and will receive her PhD from Texas Tech University in Applied Mathematics. Nusrat’s research interests include utilizing mathematical models for infectious and vector-borne diseases to effectively mitigate their impact on public health through management strategies and developing mathematical models to forecast the effects of climate change on population dynamics.Advisory Faculty
 Dr. Ron Gimbel, Director of Clemson Rural Health, Professor
Dr. Ron Gimbel, Director of Clemson Rural Health, Professor
Dr. Ronald Gimbel is a Professor in the Department of Public Health Sciences at Clemson University and Director of Clemson Rural Health. He received his PhD from the State University of New York at Albany in Public Administration and Policy and a Master of Arts degree from Webster University in Management. The Clemson Rural Health organization operates rural health clinics, a fleet of mobile health units, telehealth services, and other technologies to enhance overall wellness in South Carolina communities. Dr. Gimbel’s research focuses on improving health equity and outcomes in rural and underserved communities within an effort to bridge biomedical research with communities. Dr. Sarah Griffin, Interim Department Chair, Professor
Dr. Sarah Griffin, Interim Department Chair, Professor
Dr. Sarah Griffin is a Professor and the Interim Department Chair in the Department of Public Health Sciences at Clemson University. She received her PhD in Public Health and a Master of Public Health in Health Promotion, Education, and Behavior degrees from the University of South Carolina. She is a health researcher with extensive community-based research experience and expertise in implementation research. Dr. Griffin's research is focused on eliminating health disparities by researching the efficacy and effectiveness of complex interventions to improve health. She often uses mixed-method approaches to assess the effectiveness of community, clinical, and school based interventions addressing health equity in South Carolina. Currently, Dr. Griffin serves as Co-PI for a Centers for Disease Control and Prevention obesity prevention initiative with rural health extension. Dr. Alain Litwin, Professor
Dr. Alain Litwin, Professor
Dr. Alain Litwin is a Professor of Medicine at the University of South Carolina School of Medicine Greenville, a Professor at Clemson University School of Health Research, executive director of the Addiction Medicine Center at Prisma Health, and co-chair of the Prisma Health Opioid Stewardship Council. He received his MD from Tulane University School of Medicine and specializes in internal and addiction medicine. His research is focused on developing and studying models of Hepatitis C care for drug users and advocating for increasing access to effective care for patients. Through his roles, Dr. Litwin has helped shape public policy through collaboration with community and government organizations to develop clinical guidelines and expand access to treatments. Dr. Gary Machlis, Professor
Dr. Gary Machlis, Professor
Dr. Gary Machlis is a Professor of Environmental Sustainability in the Department of Parks, Recreation and Tourism Management at Clemson University. He received his PhD from Yale University in Human Ecology and his MS from the University of Washington in Forestry. His research interests are disaster response, science during crisis, conservation science and politics, and sustainability. Dr. Machlis has lent his expertise to multiple roles serving communities during crises, including Science Advisor to the Director of the U.S. National Park Service, co-Leader of the U.S. Department of the Interior’s Strategic Sciences Group, and an executive councilman of the National Academics of Sciences, Engineering, and Medicine Response and Resilient Recovery Strategic Science Initiative. He has created an international presence, conducting research and promoting science capacity in China, the Galapagos Islands, Haiti, Kenya, and Eastern Europe.Affiliated Faculty
 Dr. Kathleen Cartmell, Associate Professor
Dr. Kathleen Cartmell, Associate Professor
Dr. Kathleen Cartmell is an Associate Professor in the Department of Public Health Sciences at Clemson University. She received her PhD from the Medical University of South Carolina in Health and Rehabilitation Sciences and a Master of Public Health degree from the Emory University Rollins School of Public Health. She is a health services researcher with a focus on dissemination and implementation of evidence-based strategies for disease prevention and control, including interventions to optimize vaccination at the health system and community levels. She now leads a statewide multi-level intervention designed to increase HPV vaccination in South Carolina. Dr. Delphine Dean, Professor
Dr. Delphine Dean, Professor
Dr. Delphine Dean is a Ron and Jane Lindsay Family Innovation Professor in the Department of Bioengineering at Clemson University. She received her PhD and Master of Engineering degrees from the Massachusetts Institute of Technology in Electrical Engineering and Computer Science. She is the director and founder of the Clemson Center for Innovative Medical Devices and Sensors and the Research Education in Disease Diagnosis and Intervention (REDDI) Lab, which includes Clemson's only CLIA certified diagnostic laboratory, and is key in surveillance of COVID-19. She recently served as Project Lead for an NIH award aimed at sequencing all the positive samples from the REDDI Lab for surveillance of emerging strains. Dr. David Freedman, Department Chair, Professor
Dr. David Freedman, Department Chair, Professor
David L. Freedman is a professor in the Department of Environmental Engineering and Earth Sciences at Clemson University; he also serves as the Department Chair. He received his Ph.D. in Environmental Engineering from Cornell University. Dr. Freedman has received research support from SERDP, ESTCP, EPA, US DOE, US Army Construction Engineering Research Laboratory, US Air Force Office of Scientific Research, Westinghouse Savannah River Corporation, Battelle, and numerous consulting firms. The main focus of Dr. Freedman’s research is biotic and abiotic degradation of groundwater contaminants. He also has teaching and research experience with wastewater treatment systems. During the COVID pandemic, Dr. Freedman led a team that collected data on the prevalence of SARS-CoV-2 in wastewater from three sewer sheds in the Clemson area. The surveillance data was used to develop an SEIR model that predicts the numbers of infected individuals. Similar studies are envisioned for other public health issues that can be monitored using wastewater, including the prevalence of opioids. Dr. Natasha Malmin, Assistant Professor
Dr. Natasha Malmin, Assistant Professor
Dr. Natasha Malmin is an Assistant Professor in the School of Public Health at Georgia State University. She received a joint PhD in Public Policy from Georgia Institute of Technology and Georgia State University and an MPH from Emory University. Prior to her career in academia, she served as a health scientist at the Centers for Disease Control and Prevention for seven years. Areas of specialization include public health emergency response, school recovery after disasters, administrative burden and federal disaster recovery, participatory geographic information systems mapping, and community resilience. Dr. Rachel Mayo, Associate Dean for Research and Graduate Studies, Professor
Dr. Rachel Mayo, Associate Dean for Research and Graduate Studies, Professor
Dr. Rachel Mayo is a Professor in the Department of Public Health Sciences and an Associate Dean for Research and Graduate Studies in the College of Behavioral, Social and Health Sciences at Clemson University. Her recent research focuses on delivery of care to Latino patients, experiences with cancer among African Americans, and promotion of participation in breast and cervical cancer screenings among minority populations. Dr. Mayo’s research and evaluation of treatment for newborns with Neonatal Abstinence Syndrome has transformed healthcare research in communities across South Carolina. Her participation on state and national boards, such as the Alliance for a Healthier South Carolina’s Health Disparities Task Force, and Academy Health’s Health Disparities Interest group, have led to a shaping of community and public policy. Dr. Christopher McMahan, Associate Professor, Associate Director for Graduate Studies
Dr. Christopher McMahan, Associate Professor, Associate Director for Graduate Studies
Dr. Christopher McMahan is an Associate Professor and the Associate Director for Graduate Studies in the School of Mathematical and Statistical Sciences at Clemson University. He received his PhD from the University of South Carolina in Statistics and a Master of Science degree from Western Kentucky University in Mathematics. Dr. McMahan has extensive expertise in machine learning and artificial intelligence applications, COVID-19 modeling, and disease mapping and forecasting. During the 2020-2021 academic year, Dr. McMahan was a member of the public health strategy team which provided public health guidance to Clemson University amid the COVID-19 pandemic. In 2022, Dr. McMahan was named an American Statistical Association Fellow, one of the highest honors for statisticians, due to his exceptional contributions to statistical science, collaboration with researchers internationally, and promotion of scientific discovery across disciplines.Graduate Assistants
 Iromi Jayawardena, Graduate Research Assistant
Iromi Jayawardena, Graduate Research Assistant
Iromi Jayawardena is a Graduate Research Assistant in the Department of Public Health Sciences at Clemson University. She received her Master of Science degree from Sam Houston State University in Statistics and is currently a PhD student in the Applied Health Research and Evaluation program at Clemson University. Her primary research projects focus on COVID-19 vaccination and the use of data-driven approaches for vaccination uptake in communities in South Carolina through mobile health clinics. Abass Babatunde, Graduate Research Assistant
Abass Babatunde, Graduate Research Assistant
Abass Babatunde is a Graduate Research Assistant in the Department of Public Health Sciences at Clemson University. He is currently a PhD student in the Applied Health Research and Evaluation program at Clemson University. His research interests include use of public health data to evaluate and guide health intervention to ensure the optimum use of resources, especially in preventing and mitigating poor health outcomes while maintaining equity in access to care and treatment. He has worked in many capacities with international non-governmental agencies and research institutes in community health intervention design, evaluation, and management. Bonnie Treado, Graduate Research Assistant
Bonnie Treado, Graduate Research Assistant
Dr. Bonnie Treado is a Graduate Research Assistant in the Department of Public Health Sciences at Clemson University and with Clemson Rural Health and a board-certified AANP family nurse practitioner. She is currently a PhD student in the Applied Health Research and Evaluation program at Clemson University. She received her DNP and a Master’s degree in Nursing from the Medical University of South Carolina. Dr. Treado has expanded her clinical experience with patients with HIV/AIDs, immigrant communities, and rural populations of South Carolina to develop primary research interests in dissemination and implementation strategies to reduce health disparities in marginalized populations, to optimize health-related communication, and to build capacity within health systems to address community needs. Tanvir Ahammed, Graduate Research Assistant
Tanvir Ahammed, Graduate Research Assistant
Tanvir Ahammed is a Graduate Research Assistant in the Department of Public Health Sciences at Clemson University. He received his Master of Science degree in Statistics from Shahjalal University of Science & Technology in Bangladesh and is currently a PhD student in the Applied Health Research and Evaluation program at Clemson University. His primary research focuses on the application of statistical methodology to public health, including estimation of infectious disease epidemiology.Collaborators
Dr. Kerry Sease
Dr. Zichen Ma
-
Projects
CURRENT PROJECTS
1) Disease Modeling and Analytics to inform outbreak Prevention, Response, Intervention, Mitigation, and Elimination in South Carolina (DMA-PRIME)
Funder: Centers for Disease Control and Prevention/Center for Forecasting and Outbreak Analytics
Narrative: The purpose of the DMA-PRIME initiative is to save lives by increasing the ability of public health organizations and communities to prepare for, and respond to, infectious disease outbreaks through a multi-pronged approach: 1) procurement of informative data sources and their integration into proven infectious disease forecasting and outbreak analytic tools, 2) integration of these analytic tools into decision-support toolkits to inform public health response, and 3) enhancement of methods for visualizing data and communicating analytic results to decision makers and communities. This project is in close collaboration with our four implementing partners, comprising South Carolina’s (SC’s) two largest health care systems, Prisma Health and Medical University of South Carolina; Clemson Rural Health; and SC’s Center for Rural and Primary Healthcare, and in collaboration with SC’s Department of Health and Environmental Control (SCDHEC).
The decision-making toolkits will be pilot tested in real-world settings for informing a) field-level interventions for testing, treatment, and vaccination, b) healthcare system and statewide disaster planning and response, and c) community awareness on individual risk and availability of healthcare services. Ultimately, the DMA-PRIME initiative aims to integrate innovative analytic approaches to inform and improve preparedness, response, intervention, mitigation, and elimination of infectious disease outbreaks. Utilizing the strong relationships and trust cultivated between our partners throughout SC, our long-term objective is to broaden public health response to current and future infectious disease threats.
Impact: The DMA-PRIME initiative will drastically improve real-time infectious disease outbreak response by supporting always-on data collection, outbreak detection, and forecasting mechanisms for swift integration into public health response. This will be made possible by a statewide collaboration of health systems, health departments, and academic institutions with a strong working history and an enhanced ability to rapidly collect and provide data in real-time. Because healthcare systems are a major frontline defense for outbreaks, successful integration of our decision-support toolkits has potential to save thousands of lives through improving public health response, including timely delivery of essential resources to populations of greatest risk and need. Simultaneously, the public version of our toolkit will improve health outcomes through increasing understanding of individual risk and informing availability of community health care resources.
Reference: Centers for Disease Control and Prevention NU38FT000011 (PI: Lior Rennert): “Disease Modeling and Analytics to inform Outbreak Preparedness, Response, Intervention, Mitigation, and Elimination in South Carolina (DMA-PRIME)”, $17,370,990. 09-30-2023 to 09-29-2028.
2) Data-Driven Approaches for Opioid Use Disorder Treatment, Recovery, and Overdose Prevention in Rural Communities via Mobile Health Clinics and Peer Support Services
Funder: National Institutes of Health/National Institute on Drug Abuse
Narrative: This proposal will develop, deliver, and evaluate an innovative 1) Peer Support Specialist (PSS) intervention to increase Medications for Opioid Use Disorder (MOUD) initiation and retention rates in rural populations and underserved communities and 2) dynamic modeling framework to prioritize at-risk communities for delivery of Mobile Health Clinics. In collaboration with key stakeholders, the interventions will be developed in the R61 phase and implemented in the R33 phase to systematically deliver Mobile Health Clinics with PSS services to the highest priority communities in South Carolina (identified via modeling). With opioid overdose deaths continuing to rise in South Carolina (SC) and nationally, our sustainable framework has potential to prevent hundreds to thousands of opioid overdoses in SC and can be scaled up in other regions to save many more lives.
Impact: Development of a Peer Support Specialist intervention delivered by Mobile Health Clinics via our proposed framework has potential to prevent hundreds to thousands of opioid overdoses in SC alone and has potential to be scaled up and prevent many more deaths if adopted by public health decision makers in other regions or for other substances.
Reference: National Institute on Drug Abuse of the National Institutes of Health R61DA059892 (PI: Lior Rennert): “Data-Driven Approaches for Opioid Use Disorder Treatment, Recovery, and Overdose Prevention in Rural Communities via Mobile Health Clinics and Peer Support Services”, $5,546,082. 09-30-2023 to 09-29-2029.
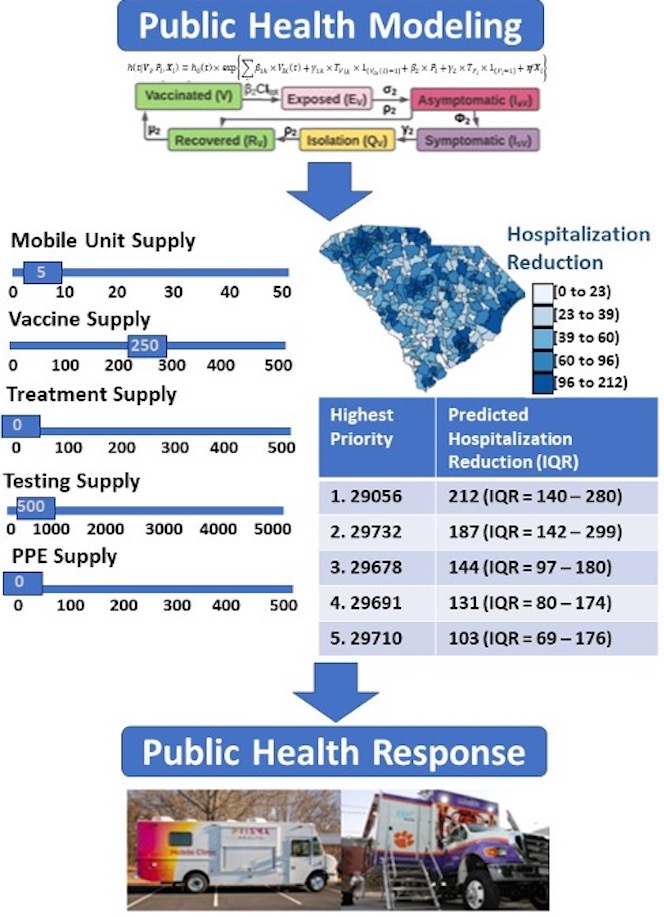
3) Developing a dynamic modeling framework for surveillance, prediction, and real-time resource allocation to reduce health disparities during Covid-19 and future pandemics
Reference: National Institutes of Health/National Library of Medicine
Narrative: This proposal will develop a dynamic simulation modeling framework for surveillance, prediction, and real-time allocation of essential resources to underserved communities in order to reduce health disparities during Covid-19 and future pandemics. Our flexible modeling framework will integrate real-time data on infectious disease outcomes with individual and community level contextual factors to inform infectious disease surveillance and improve understanding of disease epidemiology in underserved communities, and to support the decision-making process for resource allocation to high-risk populations. In collaboration with public health decision-makers, we will utilize our toolkit to inform real-time scheduling of South Carolina’s fleet of Covid-19 mobile vaccination clinics to underserved communities across the state; this has potential to save countless lives during the Covid-19 pandemic and will lay the foundation for effective resource allocation to underserved communities in other health emergencies.
Impact: Our proposal will improve pandemic planning by developing the modeling infrastructure for infectious disease surveillance and understanding of disease epidemiology in underserved communities, ultimately improving timely delivery of essential resources to those of greatest need. Utilization of this toolkit by public health decision makers can prevent thousands of future Covid-19 deaths. Through adaptation of input data sources, our modeling framework is easily translatable to other infectious diseases and geographic regions and has potential to save many more lives in future health emergencies.
Reference: National Library of Medicine of the National Institutes of Health R01LM014193 (PI: Lior Rennert): “Developing a dynamic modeling framework for surveillance, prediction, and real-time resource allocation to reduce health disparities during Covid-19 and future pandemics,” $3,092,665. 01-05-2023 to 11-30-2028.
PREVIOUS PROJECTS
Data-driven approach to identify high-risk rural communities for delivery of mobile health clinics
Our team is developing and implementing a modeling framework to identify communities at greatest risk of OUD, hepatitis C virus (HCV), and human deficiency virus (HIV) for delivery of mobile health clinics. We are working with South Carolina’s Center for Rural and Primary Health Care, Clemson Rural Health, and Prisma Health to identify high-risk rural communities for targeted delivery of Mobile Health Clinics.Evaluation of policies limiting opioid exposure
In a joint collaboration between Prisma Health’s Opioid Stewardship Program and Clemson University, our teams are continuously evaluating the immediate impact and downstream effects of policies limiting opioid exposure. Importantly, we have found that policies implemented by Prisma Health, and the State of South Carolina, have successfully limited opioid exposure without compromising patient pain and discomfort.Statewide infectious disease surveillance, prediction, and resource allocation
Our team is working on developing a dynamic simulation modeling framework for surveillance, prediction, and real-time allocation of essential resources to underserved communities in order to reduce health disparities during Covid-19 and future pandemics. Our flexible modeling framework will integrate real-time data on infectious disease outcomes with individual and community level contextual factors to inform infectious disease surveillance and improve understanding of disease epidemiology in underserved communities, and to support the decision-making process for resource allocation to high-risk populations. The proposed modeling toolkit will help inform and assist the distribution of Covid-19 mobile health clinics to medically underserved and at-risk communities.Infectious disease Epidemiology
Understanding infectious disease epidemiology is critical for understanding individual and community risk, conducting accurate disease surveillance, and implementing effective mitigation measures. This knowledge is especially useful to estimate input parameters of modeling frameworks used to allocate resources to at-risk communities. Using statistical models, we have estimated a wide range of Covid-19 epidemiological metrics, including risk of reinfection, vaccine effectiveness and waning immunity, and predictive value of clinical symptoms.Covid-19 Modeling for Institutes of Higher Education
Our team is developing an integrative modeling toolkit for Covid-19 surveillance, prediction, resource allocation, and intervention evaluation in institutes of Higher Education. Our goal is to generalize this toolkit in other institutional settings in order to inform public health decision making. This toolkit has been utilized at Clemson University to inform decision making on a wide variety of mitigation measures (e.g., testing strategies) and procurement of essential resources.Utilizing wastewater surveillance for early disease detection and response
Utilizing samples collected through wastewater, our team has developed dynamic models to predict active Covid-19 cases in local communities. Currently, we are working to expand wastewater detection to detect communities at high-risk for opioid overdose. The ultimate goal of this project is to supplement resource allocation models with this information to increase the timeliness and effectiveness of mobile health clinic response, community response, and educational efforts.Building a campus-community partnership to raise public health awareness
With funding from the Interfaith Youth Core and FIVA Carolinas, we have built a partnership with 60 African-American churches in order to raise Covid-19 vaccine awareness and distribute other Covid-related information.Identifying predictors of cognitive decline in older adults
Our team is working on an extensive examination of the relationship between cognitive reserve built up through life experiences and cognitive decline in older adults. The ultimate goal is to help identify influential factors of cognitive decline and potential timing for early interventions to promote cognitive health in older adults. -
Research Publications
Rennert L,† Howard KA,† Kickham CM, Gezer F, Coleman A, Roth P, Boswell K, Gimbel RW, Litwin AL. Implementation of a mobile health clinic framework for Hepatitis C virus screening and treatment: a descriptive study. Lancet Reg Health - Americas. 2024;29:100648. https://doi.org/10.1016/j.lana.2023.100648. † Denotes co-first author
Howard KA, Massimo L, Griffin SF, Gagnon RJ, Zhang L, Rennert L. Systematic examination of methodological inconsistency in operationalizing cognitive reserve and its impact on identifying predictors of late-life cognition. BMC Geriatr. 2023;23(1):547. https://doi.org/10.1186/s12877-023-04263-9
Rennert L, Ma Z. An Epidemiological Modeling Framework to Inform Institutional-Level Response to Infectious Disease Outbreaks: A Covid-19 Case Study. Revision Invited (Nature Scientific Reports); 2023. https://doi.org/10.21203/rs.3.rs-3116880/v1
Gezer F, Howard KA, Litwin AH, Martin NK, Rennert L. Identification of Factors Associated with, and Prediction of, Opioid- and HCV-Related Hospitalizations at the Zip Code Level: A Statistical Modeling Approach. Revision Invited (Lancet Public Health). SSRN; 2023. https://doi.org/10.2139/ssrn.4506562
Hossfeld C, Rennert L, Baxter SLK, Griffin SF, Parisi M. The Association between Food Security Status and the Home Food Environment among a Sample of Rural South Carolina Residents. Nutrients. 2023;15(18):3918. https://doi.org/10.3390/nu15183918
Babatunde A, Rennert L, Walker KB, Furmanek DL, Blackhurst DW, Cancellaro VA, Litwin AH, Howard KA. Association between Initial Opioid Prescription and Patient Pain with Continued Opioid Use among Opioid-Naïve Patients Undergoing Elective Surgery in a Large American Health System. Int J Environ Res Public Health. 2023;20(10):5766. https://doi.org/10.3390/ijerph20105766
Rennert L, Ma Z, McMahan CS, Dean D. Covid-19 vaccine effectiveness against general SARS-CoV-2 infection from the omicron variant: A retrospective cohort study. Katoto PD, editor. PLOS Glob Public Health. 2023;3(1):e0001111. https://doi.org/10.1371/journal.pgph.0001111
Rennert L, Howard KA, Walker KB, Furmanek DL, Blackhurst DW, Cancellaro VA, Litwin AH. Evaluation of policies limiting opioid exposure on opioid prescribing and patient pain in opioid-naive patients undergoing elective surgery in a large American health system. J Patient Saf. 2022. https://doi.org/10.1097/PTS.0000000000001088
Rennert L, Ma Z, McMahan CS, Dean D. Effectiveness and protection duration of Covid-19 vaccines and previous infection against any SARS-CoV-2 infection in young adults. Nat Commun. 2022;13(1):3946. https://doi.org/10.1038/s41467-022-31469-z
McMahan CS, Lewis D, Deaver JA, Dean D, Rennert L, Kalbaugh CA, Shi L, Kriebel D, Graves, D, Popat SC, Karanfil T, Freedman DL. Predicting COVID-19 infected individuals in a defined population from wastewater RNA data. ACS EST Water. 2022;2(11):2225–32. https://doi.org/10.1021/acsestwater.2c00105
Kunkel D, Stuenkel M, Sivaraj LB, Colenda CC, Pekarek L, Rennert L. Predictive value of clinical symptoms for COVID-19 diagnosis in young adults. J Am Coll Health. 2022;1–4. https://doi.org/10.1080/07448481.2022.2068963
King KL, Wilson S, Napolitano JM, Sell KJ, Rennert L, Parkinson CL, Dean D. SARS-CoV-2 variants of concern Alpha and Delta show increased viral load in saliva. Abd El-Aty AM, editor. PLOS ONE. 2022;17(5):e0267750. https://doi.org/10.1371/journal.pone.0267750
Pericot-Valverde I, Heo M, Niu J, Rennert L, Norton BL, Akiyama MJ, Arsten J, Litwin AH. Relationship between depressive symptoms and adherence to direct-acting antivirals: Implications for Hepatitis C treatment among people who inject drugs on medications for opioid use disorder. Drug Alcohol Depend. 2022;234:109403. https://doi.org/10.1016/j.drugalcdep.2022.109403
Rennert L, McMahan CS. Risk of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) reinfection in a university student population. Clin Infect Dis. 2022;74(4):719–22. https://doi.org/10.1093/cid/ciab454
Plumb EV, Ham RE, Napolitano JM, King KL, Swann TJ, Kalbaugh CA, Rennert L, Dean D. Implementation of a rural community diagnostic testing strategy for SARS-CoV-2 in Upstate South Carolina. Front Public Health. 2022;10:858421. https://doi.org/10.3389/fpubh.2022.858421
Gormley MA, Akiyama MJ, Rennert L, Howard KA, Norton BL, Pericot-Valverde I, Muench S, Heo M, Litwin AH. Changes in health-related quality of life for Hepatitis C Virus–infected people who inject drugs while on opioid agonist treatment following sustained virologic response. Clin Infect Dis. 2022;74(9):1586–93. https://doi.org/10.1093/cid/ciab669
McMahan CS, Self S, Rennert L, Kalbaugh C, Kriebel D, Graves D, Colby C, Deaver JA, Popal SC, Karanfil T, Freedman DL. COVID-19 wastewater epidemiology: A model to estimate infected populations. Lancet Planet Health. 2021;5(12):e874–81. https://doi.org/10.1016/S2542-5196(21)00230-8
Rennert L, Kalbaugh CA, McMahan CS, Shi L, Colenda CC. The impact of phased university reopenings on mitigating the spread of COVID-19: A modeling study. BMC Public Health. 2021;21(1):1520. https://doi.org/10.1186/s12889-021-11525-x
Massimo L, Rennert L, Xie SX, Olm C, Bove J, Van Deerlin V, Irwin DJ, Grossman M, McMillan CT. Common genetic variation is associated with longitudinal decline and network features in behavioral variant frontotemporal degeneration. Neurobiol Aging. 2021;108:16–23. https://doi.org/10.1016/j.neurobiolaging.2021.07.018
Howard KA, Rennert L, Pericot-Valverde I, Heo M, Norton BL, Akiyama MJ, Agyemang L, Litwin AH. Utilizing patient perception of group treatment in exploring medication adherence, social support, and quality of life outcomes in people who inject drugs with Hepatitis C. J Subst Abuse Treat. 2021;126:108459. https://doi.org/10.1016/j.jsat.2021.108459
Rennert L, McMahan CS, Kalbaugh CA, Yang Y, Lumsden B, Dean D, Pekarek L, Colenda CC. Surveillance-based informative testing for detection and containment of SARS-CoV-2 outbreaks on a public university campus: An observational and modelling study. Lancet Child Adolesc Health. 2021;5(6):428–36. https://doi.org/10.1016/S2352-4642(21)00060-2
Heo M, Pericot-Valverde I, Rennert L, Akiyama MJ, Norton BL, Gormley M, Agyemand L, Arnsten JH, Litwin AH. Hepatitis C Virus direct-acting antiviral treatment adherence patterns and sustained viral response among people who inject drugs treated in opioid agonist therapy programs. Clin Infect Dis. 2021;73(11):2093–100. https://doi.org/10.1093/cid/ciab334
Rennert L, Heo M, Litwin AH, Gruttola VD. Accounting for confounding by time, early intervention adoption, and time-varying effect modification in the design and analysis of stepped-wedge designs: application to a proposed study design to reduce opioid-related mortality. BMC Med Res Methodol. 2021;21(1):53. https://doi.org/10.1186/s12874-021-01229-6
Charron E, Rennert L, Mayo RM, Eichelberger KY, Dickes L, Truong KD. Contraceptive initiation after delivery among women with and without opioid use disorders: A retrospective cohort study in a statewide Medicaid population, 2005–2016. Drug Alcohol Depend. 2021;220:108533. https://doi.org/10.1016/j.drugalcdep.2021.108533
Pericot‐Valverde I, Rennert L, Heo M, Akiyama MJ, Norton BL, Agyemang L, Lumsden B, Litwin AH. Rates of perfect self‐reported adherence to direct‐acting antiviral therapy and its correlates among people who inject drugs on medications for opioid use disorder: The PREVAIL study. J Viral Hepat. 2021;28(3):548–57. https://doi.org/10.1111/jvh.13445
Rennert L, Kalbaugh CA, Shi L, McMahan CS. Modelling the impact of presemester testing on COVID-19 outbreaks in university campuses. BMJ Open. 2020;10(12):e042578. https://doi.org/10.1136/bmjopen-2020-042578
